About Epicutaneous Tests By Dr. Rose Private Hospital In Budapest
- 25 Jun 2021 12:51 PM
The exact definition is complicated by the fact that most of our allergenic substances consist of several ingredients, and it is rare for accurate information to be available about each ingredient.
The most important information about the epicutaneous test is summarized here by Prof. Dr. Kristóf Nékám, an allergologist at Dr. Rose Private Hospital.
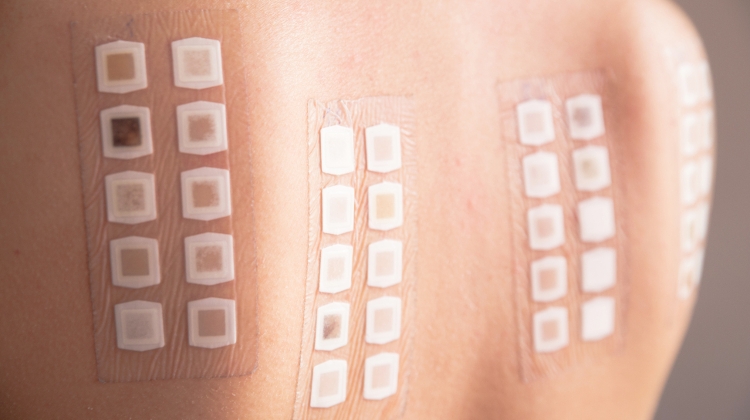
Detection of allergens is most effective when the diagnostic procedure replicates real life. Epicutaneous tests are accordingly superficial skin tests, which means that (usually) several substances - possibly in different concentrations - are applied to the patient's skin in appropriate patches and at different times we check for any local symptoms, hives, or eczema at the site of application.
The test itself is recommended for essentially any persistent, usually itchy, often moist skin symptoms - many patients can also identify the trigger (e.g., washing powder) based on its location.
The small area of skin under the patches is examined from 15 minutes to one week after application (because depending on the material and the patient's reaction, local symptoms are expected to appear between these time limits, which may decrease in intensity or persist for days).
Typically, it involves applying more than ten possible allergens, based on medical history data. With literally thousands of allergenic compounds around the world, ’standard lines’ were compiled in the 1950s according to the frequency of symptomatic elements.
These can be specific to the given country or continent (so there is a ’Hungarian’ standard series or a ’European’ series - these differ in some materials) – and there is also a smaller series of elements for when the source of the symptom-causing substance(s) is observed by the patient as probable (e.g., ’dental line’, ’photographic chemicals line’, or ’hairdressing chemicals line’).
If, in the case of the ’positivity’ found in the study (in addition to the positivity of the control) - even just one - often difficult to answer questions remain: where, when, and under what circumstances is the patient related to the given substance or substances, and can this relationship be permanently eliminated for asymptomatic purposes?
It is common experience, nevertheless, that symptoms do not disappear completely, usually because there are hundreds of products in our environment that have components that are only partially similar to one of the elements in the line and which may be enough to cause symptoms, though even identifying them in the patient's lifestyle can be an unsolvable task.
Ultimately, strict avoidance of the product(s) can usually bring improvement/asymptomatic relief to the patient, but most often topical or oral medications are also involved.
Thus, the test itself is performed with strips of the test substance (always only one) adhered to the patient's back without damaging the skin, which remain on the patient's skin for 24 hours.
During this time, the skin cannot be affected in any way (i.e., not even with water).
In the first hour after application, usually at 20-40-60 minutes, by lifting the strips the possibility of ’early’ reactions is examined (these are always glued back afterwards), then after 24-48, possibly 72 hours, or even after a week in the absence of reactions.
The latter two test times are used if there are no (usually itchy) lesions at either application site at 48 hours.
Until the test strips are removed, the affected skin must not be exposed to water or other substances, after which water is permitted, but not skin care products or medicines before the end of the test.
When discussing the test, the treating physician should be informed about any topical or oral medication because, for example, antihistamines or steroids reduce the ability to have an allergic reaction, which can lead to ’false negative’ results.
Antihistamines should not be taken for 72 hours prior to the test; even more effective steroids (a daily dose above 8 mg) may invalidate the study.
The results of the epicutaneous tests will help to identify the trigger substance or substances, and replace them with other asymptomatic substances or, in a lucky case, omit them.
Nickel is the most common cause of symptoms in Hungary.
Click here to virtually visit Dr. Rose Private Hospital



























LATEST NEWS IN current affairs